A Collaborative Approach
Achieve high quality, timely provider data

Collaborative Provider Data Management
The burden of improving provider data accuracy has fallen on contracted provider groups as health plans increase the frequency and extent of their data collection and validation efforts.
Direct outreach to physician offices by multiple health plans is not a sustainable approach to provider data maintenance. Not only does this approach bypass the management layer of provider organizations (IPA’s, health systems, MSO’s etc.), it imposes an unacceptable overhead to the physician's practice and has been proven to fail to produce the necessary data quality.
In order for health plans to achieve high quality, timely provider data without alienating their contracted providers, it is imperative that both plans and providers adopt a more collaborative approach to data collection and integration.
The Sanator Provider Registry is a collaborative data management platform leveraged by major provider organizations and health plans to reduce the administrative burden of provider data maintenance, data verification and alignment with operational processes.

Excellence in Provider Data Management
- Improved provider experience
- Directory accuracy and consumer satisfaction
- Regulatory compliance
- Improved data quality and reduced administration costs
- Insulation from evolving state and federal standards
High Performing Networks
High quality provider networks are the lifeblood of a successful health plan. Health plans partner with provider organizations to build these networks that are always looking for ways to attract and retain the best doctors, groups and facilities.
Sanator offers a provider network management (PNM) capability that enables provider organizations to optimize networks by understanding provider behaviors and characteristics that extend beyond their traditional profile.
Sanator Services
Sanator offers a suite of services for provider organizations including IPA's, MSO's, ACO's and hospital based systems.
Integrate
A Single View of Provider Data Across Systems
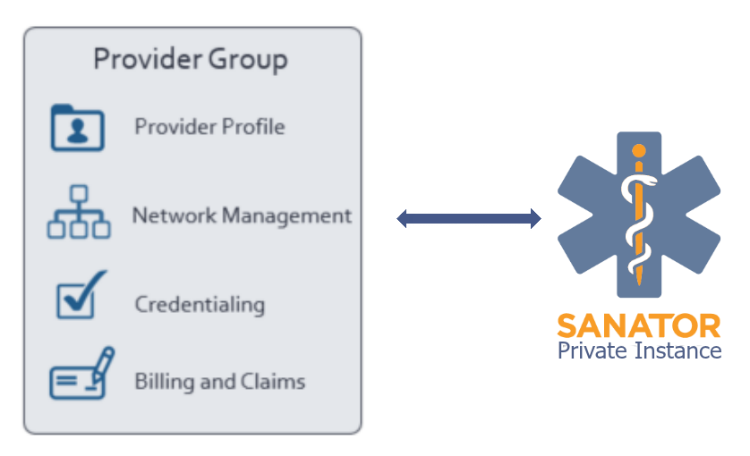
Many provider organizations (PO's) have provider data spread across multiple internal systems. This makes it difficult to produce the extracts requested by health plans or regulators for the purposes of roster validation or audit.
Sanator resolves the internal management of provider data by linking internal systems and offers a single point of data management via the Sanator portal.
- Load all internal representations of your providers into a Sanator Private Instance to create a single consolidated provider profile and cross reference of all of your internal ID’s
- Cleanse locations to USPS standards, apply geocoding
- Validate state license number, NPI and CMS Facility certification number
- Refresh data on a daily basis and receive updated provider profile data and cross reference information
Collaborate
Sanator Provider Registry
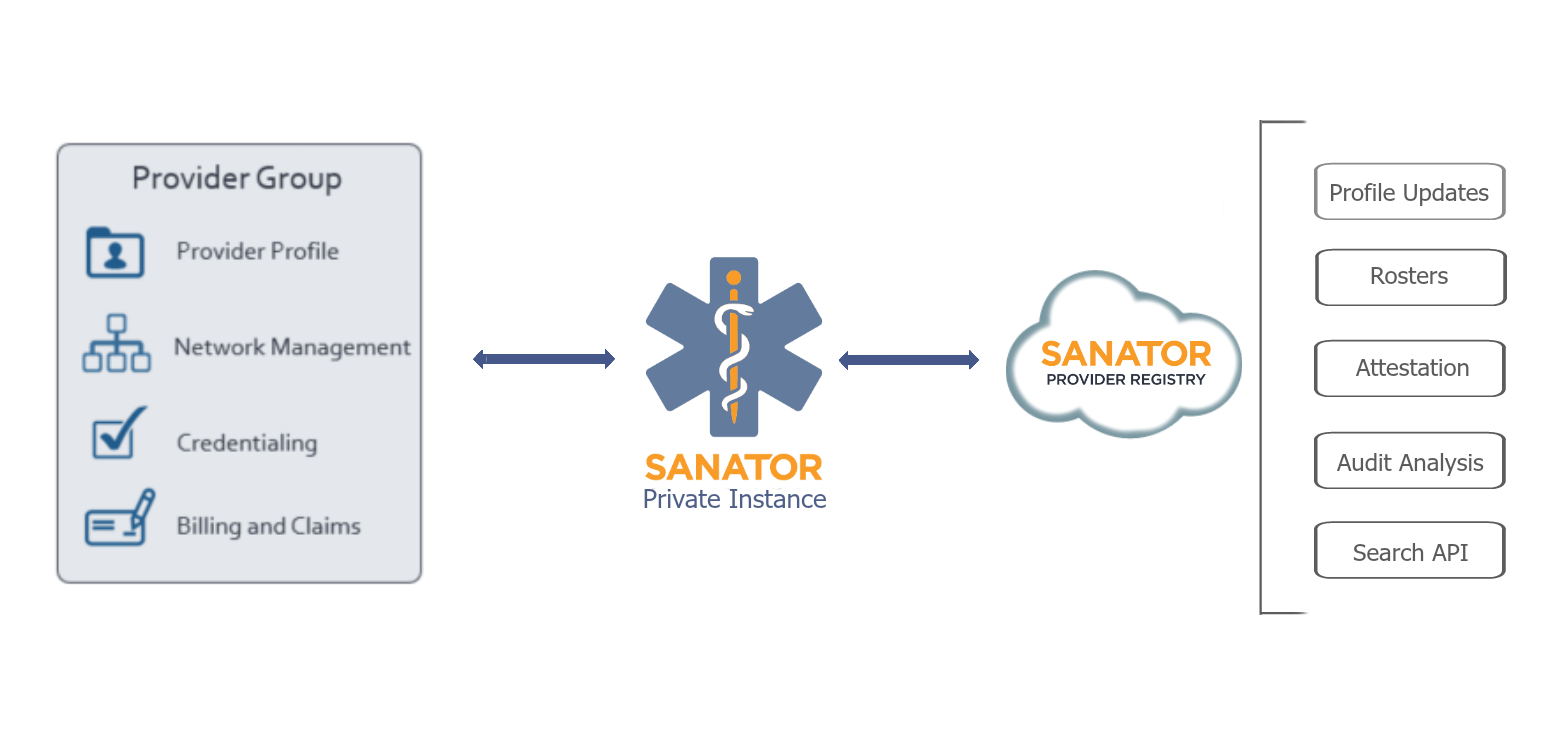
- Compare your provider data to the trusted provider profile within the Sanator Registry and receive updates and conflict notifications
- Collaborate with your peers, trade associations and health plans on the maintenance and validation of provider profiles
- Distribute updates to your provider profiles to your contracted health plans
- Automate the reconciliation of health plan rosters and the periodic attestation of provider data
- Create audit reports between your data and any contracted party to identify gaps
- Embed Sanator Search API in internal applications
Manage
Provider Portal
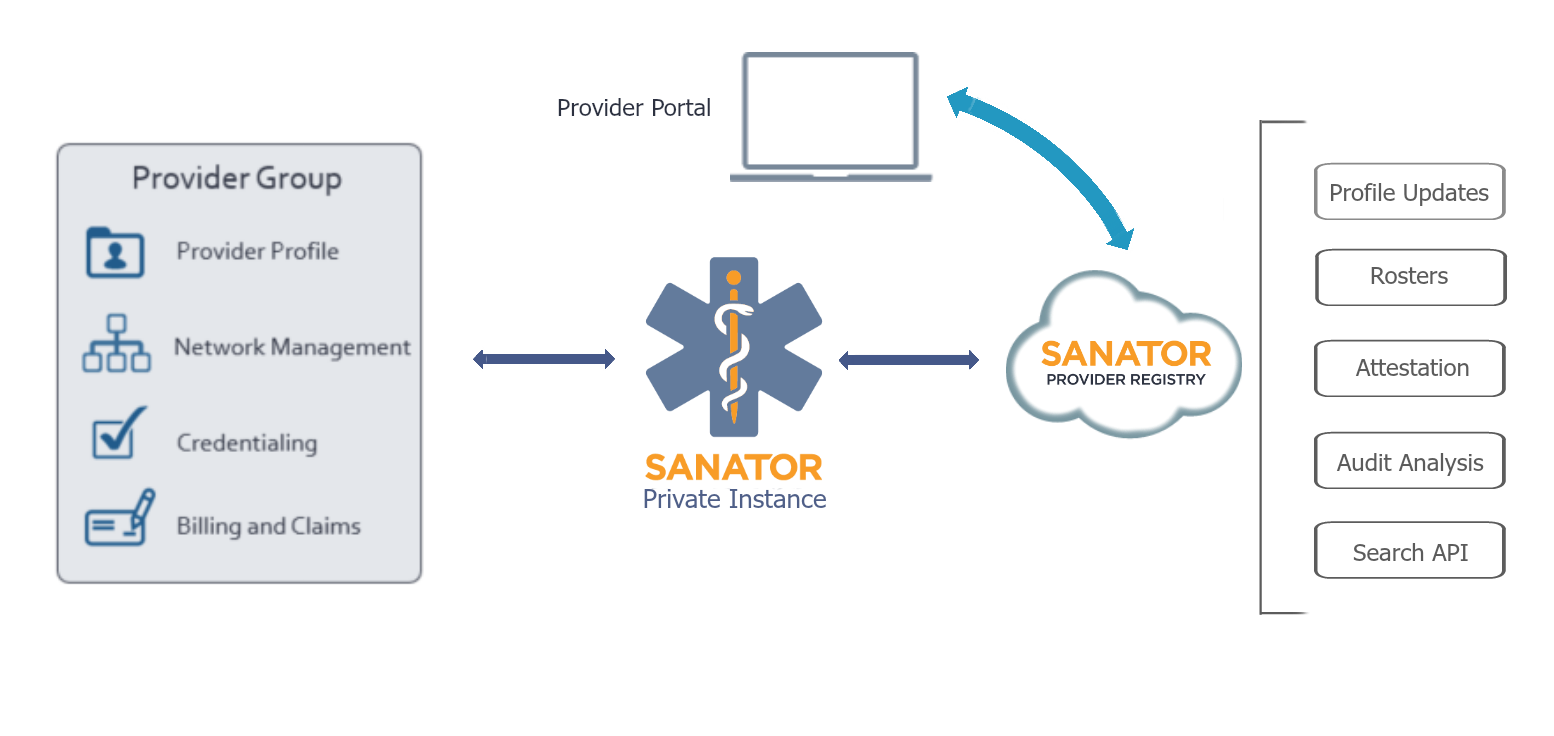
- Maintain all your provider data in a single application
- Link rosters and provider profiles to health plan contracts
- Gain insight into provider data to fill gaps in your data concerning services, provider demographics and relationships
- Manage provider profiles and the distribution of provider data as a service to your providers
Optimize
Provider Network Management
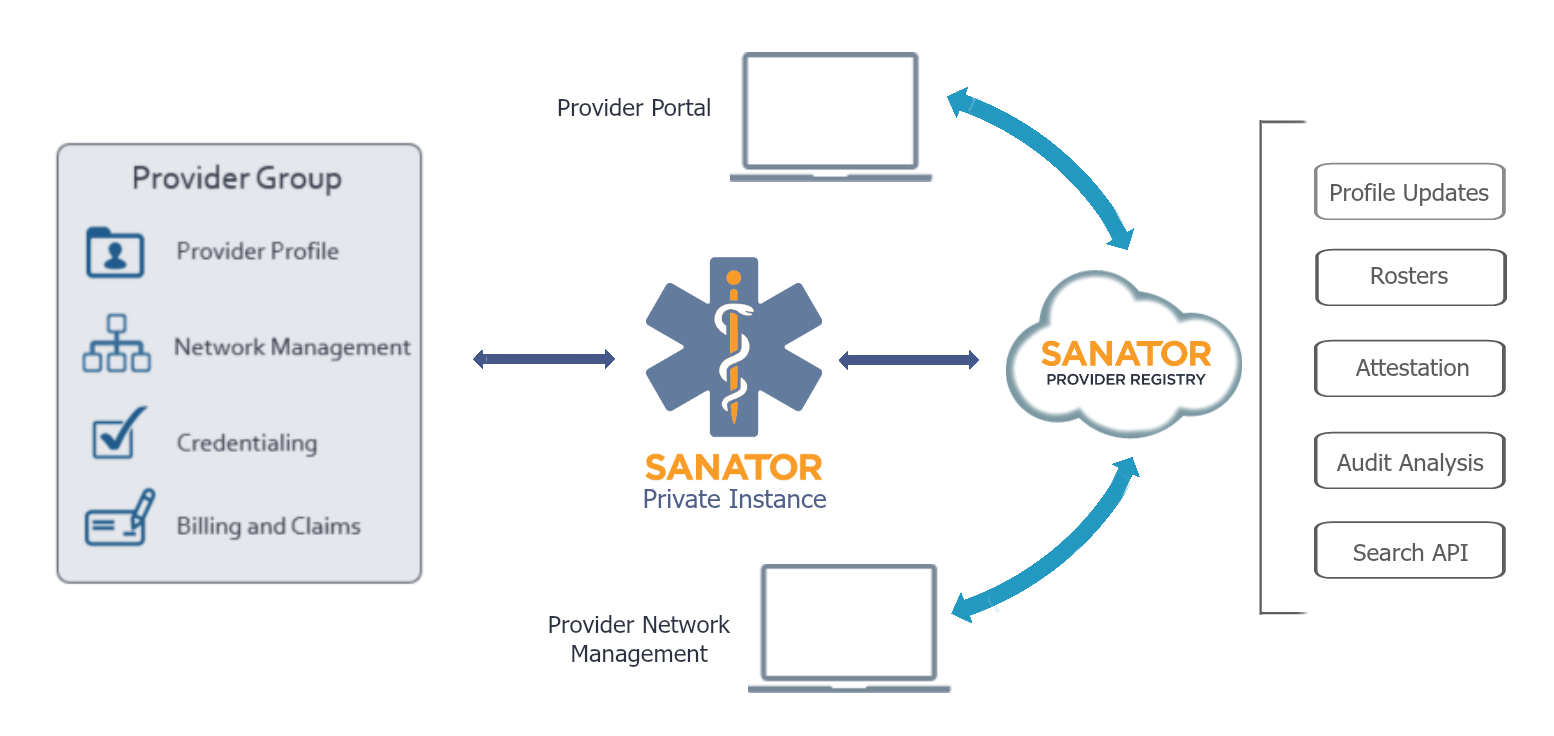
- Provider Organizations may leverage the system-wide view of providers to offer additional insight into provider utilization and commitments across groups and plans
- Sanator provides an extensive set of reports that analyze providers across plans, locations and groups.